Lucas Baumard, PhD | 27th May 2025
T follicular helper (Tfh) cells are a specialized subset of CD4+ T cells that are important for providing a “helper” function to B cells to generate long-lived antibody responses in germinal centers (GCs). Germinal centers are transient structures within B cell follicles formed by Tfh-B cell interactions, where B cells undergo affinity maturation to memory B cells and plasma cells.1 B cell follicles are specialized structures within lymphoid tissue, particularly secondary lymphoid tissues like the lymph nodes and spleen that are important sites of B cell development and antibody production.2
Tfh cells are essential immunological cells that drive healthy and long-term immune responses to infection but also protective responses (generation of long term immunity) to most human vaccines.3 However, they are also associated with autoimmune diseases such as systemic lupus erythematosus and rheumatoid arthritis.4
T follicular cells can be characterized by the surface markers they express and the cytokines they release. This guide describes markers that can be used to identify Tfh developmental stages from proto/early Tfh cells to GC Tfh cells.
Tfh cells are generally present as two distinct populations: early/ proto-Tfh cells, and final state, GC Tfh cells. These populations can be differentiated mainly by different expression patterns of chemokine receptors (Table 1).
| Marker | Early TFH | GC TFH | Naive CD4 T cell | Activated non-TFH CD4 |
|---|---|---|---|---|
| CXCL13 | +/- | — | — | — |
| CD200 | +/- | + | — | — |
| CCR7 | + | +/- | ++ | Variable |
| CXCR5 | + | ++ | — | — |
| Bcl6 | + | ++ | — | — |
| PD-1 | + | ++ | — | Variable |
| IL-21 | + | ++ | — | Variable |
| ICOS | + | + | — | Variable |
| SAP | + | ++ | + | + |
| CXCR4 | + | ++ (mRNA) | + | + |
| BTLA | + | ++ | + | +/- |
| SLAM | Unknown | + | + | Variable |
| IL-4 | — | + | — | Th2+ |
Table 1: Expression of markers for human (early) Tfh, GC Tfh and other CD4+ cells. +: positive expression, ++: high expression, +/-: low expression, —: no detectable expression. Adapted from 5
The differentiation of Tfh cells from naïve CD4+ T cells to mature GC Tfh cells requires numerous signaling factors and interactions with other cell types to stimulate migration into the B cell follicle and maturation in the germinal center. Characteristic protein markers can be used to identify Tfh cells at each stage of this progression.
Figure 1: Differentiation pathways of naïve CD4+ T cells (Th0). Transcription factors and release cytokines for each subtype are indicated. Top cytokines drive differentiation of each subtype. Type 1 immune response: defense against intracellular bacteria, protozoa and viruses; type 2: defense against helminths and venoms; type 3: defense against extracellular bacteria and fungi.
Dendritic cells (DCs) drive the differentiation of CD4+, naïve T cells into a variety of CD4+ T cell subsets: Th1, Th2, Th17, Treg and Tfh cells (Figure 1). For Tfh cells, this process is complex and not well understood. It is believed that DCs are necessary for priming of Tfh and GC initiation (Figure 2), however secondary drivers are needed to complete Tfh development – most likely further antigen-presentation dependent activation and IL-21 signalling.1
Figure 2: Tfh cell maturation. Dendritic cells present antigen to naïve T cells, inducing differentiation into various CD4+ subsets. Early Tfh destined for a final Tfh state receive secondary signals and move into the B cell zone, where they interact with B cells in germinal centers, driving B cell maturation and differentiation.
CCR7
Upon activation, early Tfh cells that express the chemokine receptor CCR7 migrate to the T cell zone of the T-B border of secondary lymphoid tissues (e.g. spleen, lymph nodes) to await final differentiation (Figure 2).6 Whilst CCR7 is not a marker of final state Tfh cells, it might be useful as a marker of early Tfh activation – CCR7hiPD-1low cells can be described as having a resting phenotype as newly activated Tfh cells begin to migrate, compared to the CCR7lowPD-1high effector phenotype of Tfh cells undergoing differentiation.7
During this CCR7+ stage, early Tfh cells are susceptible to non Tfh-associated differentiation signals within secondary lymphoid tissues, which can affect their ultimate developmental path. Depending on the cytokine signals received, Tfh cells might instead transition into another CD4+ T cell subset (Figure 2), which would lead to the cell leaving the lymphoid tissue for inflammatory sites. Early Tfh, GC Tfh and other CD4+ cell populations can be distinguished by changing expression of various surface markers, chemokines and cytokines (Table 1).
Figure 3: IHC of human spleen stained with Anti-CCR7 Antibody [ARC0231] (A307143).
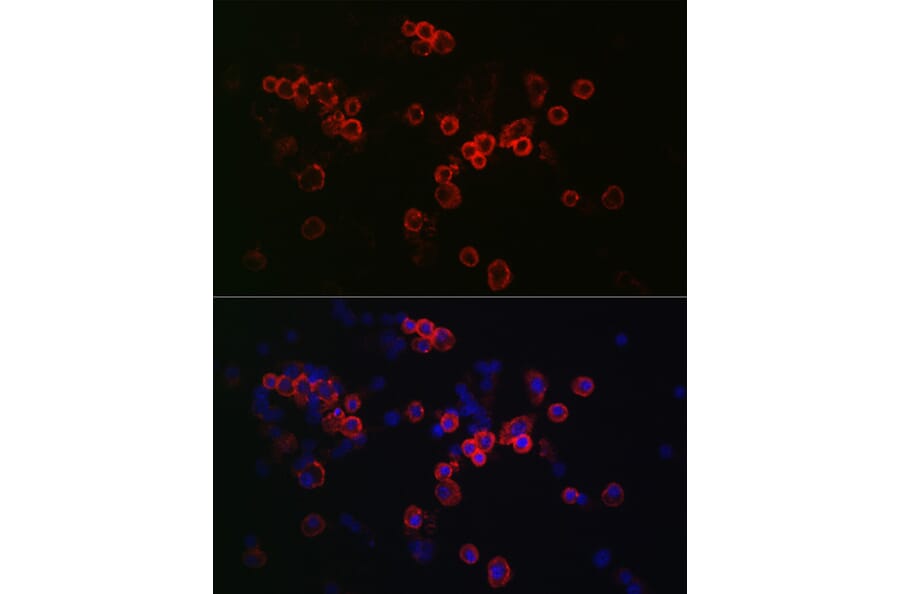
Figure 4: Immunofluorescence of RAW 264.7 cells stained with Anti-CCR7 Antibody (A89932).
ICOS
Early Tfh cells destined for a final Tfh state receive secondary signals, with IL-68 and ICOS (inducible T cell costimulator, CD278)9 shown to be important molecules in driving Tfh differentiation, whilst IL-2 can inhibit this.10
ICOS is a surface molecule sharing homologous structure and function to CD28 and is important for Tfh regulation and localization of Tfh within secondary lymphoid organs.11 ICOS binding to its ligand ICOSL and antigen presentation from DCs drives the upregulation of CXCR5 and Bcl6, another important Tfh marker, as well as downregulation of CCR7 in naïve Tfh cells (Figure 5). This drives their differentiation to GC Tfh cells and their migration from the T cell zone through the T-B border to the B cell zone (Figure 2).9 Here, Tfh cells bind B cells, which also express ICOSL, driving B cell activation and differentiation.
Figure 5: Molecular interactions between Tfh cells, dendritic cells and B cells. IL-12 is produced by dendritic cells to lead to CD4+ T cell maturation into Tfh cells by activating STAT4. This results in the production of IL21, a cytokine that acts in an autocrine way to activation STAT3, which leads to differentiation by upregulating the transcription factors Bcl6 and Ascl2. STAT3 can also be activated by other cytokines such as IL-6, produced by both dendritic and B cells. Bcl6 and Ascl2 upregulate expression of CXCR5 and downregulate CCR7, and the early Tfh cells then migrate to the T:B border. Differentiation into germinal center Tfh cells (GC Tfh cells) occurs due to further interactions with B cells (e.g. CD28–CD86, ICOS–ICOSL, PD-1– PD-1L, CD40–CD40L). Adapted from 14
More broadly, ICOS is expressed on activated (CD45RO+) CD4+ and CD8+ cells, predominantly within and around germinal centers, which may have started out as early Tfh cells before receiving non-Tfh destination signals.12 CD8+ICOS+ cells have been characterized as Tissue resident memory cells.13
CXCR5
CXCR5 is the main Tfh marker and is a chemokine receptor expressed in both early Tfh and GC Tfh cells, though expression is significantly higher in the latter (Table 1).5 It can therefore also be seen as a marker of the transition between early and GC Tfh cells. As expression of CXCR5 increases in Tfh cells, CCR7 expression decreases, reflecting the cells’ localization: CCR7 keeps them within the T cell zone of the T-B border, whilst CXCR5 drives migration of early Tfh cells to germinal centers via its ligand CXCL13. CXCR5 and ICOS expression also encourage co-localization with B cells in the B cell zone (Figure 2), which present antigen and the ICOSL to Tfh cells, necessary to maintain Tfh survival.15 These interactions ultimately form the GC, which consists of Tfh cells, B cells, macrophages, follicular dendritic cells and stroma.16
Figure 6: IHC of mouse spleen stained with Anti-CXCR5 Antibody [ARC1363] (A308772) in orange. Nuclei are marked in blue by DAPI.
Figure 7: Flow cytometry of Expi293 cells transfected with human CXCR5 (blue) or an irrelevant protein (red) stained with Recombinant Anti-CXCR5 Antibody [DMC679] (A318689).
In addition to its expression on Tfh populations, CXCR5 is also expressed on B cells and circulating Th1, Th2 and Th17 cells.17,18 These circulating Th cells most likely represent the population of naïve CD4+CXCR5+ cells that migrated to secondary lymphoid tissues and received non-Tfh determining signals (Figure 2), pushing them out of these tissues to the circulation. However, it is possible these could also represent a population of extra-follicular Tfh differentiated into T helper cells. CXCR5+ Th2 and Th17 cells can induce B cell immunoglobulin production whereas CXCR5+ Th1 cells cannot.18 CXCR5+ Tfh cells can be distinguished from CXCR5+ B cells with a co-stain for CD4.
Differentiated GC Tfh cells can be identified as CXCR5hiPD-1hiBcl6hiCCR7low and by the release of CXCL13, IL-21 and IL-4.16
Bcl6 is well-established as a lineage-defining transcription factor for Tfh cells. Tfh cells fail to develop from naïve CD4+ T cells in its absence, while Bcl6 deletion from competent Tfh cells converts them into other T cell types such as Th1 cells.19
Figure 8: IHC of human tonsil stained with Anti-Bcl-6 Antibody [BCL6/1527] (A249906).
Figure 9: Immunofluorescence of MCF-7 cells stained with Anti-Bcl-6 Antibody [PCRP-BCL6-1D3] (A277775) in green. Cell membranes are marked in red by phalloidin.
While expressed on many immune cell types, high PD-1 expression is commonly employed as a marker of Tfh cells. Like in other cells, PD-1 in Tfh cells acts as a regulatory brake to prevent excessive Tfh activity. Tfh PD-1 engages with PD-L1 on follicular B cells, and plays a role in Tfh positioning, ensuring that only T cells expressing a high level of ICOS are recruited into the GC.20
Figure 10: IHC of human tonsil stained with Recombinant Anti-PD1 Antibody [PDCD1/1410R] (A249588).
Figure 11: Flow cytometry of MCF-7 cells stained with Anti-PD1 Antibody [EH12.2H7] (APC) (A121900).
CXCL13 is a ligand for CXCR5 that acts as a B cell attracting chemokine, released by Tfh cells17 in response to Bcl6 induction.15 CXCL13 also attracts Tfh cells,21 increasing the number of Tfh cells at the site, and therefore the amount of CXCL13 released, in a positive feedback loop. By bringing Tfh and B cells into close contact, CXCL13 can drive Tfh-dependent B cell activation, mainly through T cell receptor-MHCII and CD40-CD40L binding.5
Germinal center Tfh cells have been shown to produce the cytokines IL-21 and IL-4.22 IL-4 is also released from eosinophils,23 mast cells and basophils24 and Th2 cells25 whilst IL-21 is released from natural killer cells26 and other CD4+ cells including Th17 cells.27 Mice deficient in IL-4 and IL-21 have significantly reduced B cell responses underpinning the role of the cytokines in stimulating B cell function and immunoglobulin production.28,29 Though IL-4 is also expressed in and released by other Th cells (CCR5int) within secondary lymphoid tissues, it is significantly higher in GC Tfh CCR5high cells and highly associated with IL-21, providing a means of differentiation between these subsets.15 IL-4 and IL-21 release is driven by increased expression of the transcription factor Maf in CXCR5high Tfh cells.15
T follicular cells can be examined with a variety of experimental techniques. Surface marker expression can be detected by flow cytometry, IHC or western blot. Cytokine expression can be measured by ELISA, ELISPOT or intracellular flow cytometry. Early and germinal center Tfh cells can be differentiated based on high/intermediate/low expression patterns of various surface markers as well as the release of cytokines/ chemokines.
Diagrams created with BioRender.com.


![Immunofluorescence - Anti-CCR7 Antibody [ARC0231] (A307143)](https://cdn.antibodies.com/image/category/primaries/cell-markers/A307143_4_Tfh_crop.jpg?profile=product_image)

![IHC - Anti-CXCR5 Antibody [ARC1363] (A308772)](https://cdn.antibodies.com/image/catalog/308/A308772_3.jpg?profile=product_image)
![Flow cytometry - Recombinant Anti-CXCR5 Antibody [DMC679] (A318689)](https://cdn.antibodies.com/image/catalog/318/A318689_1.jpg?profile=product_image)
![IHC - Anti-Bcl-6 Antibody [BCL6/1527] (A249906)](https://cdn.antibodies.com/image/catalog/249/A249906_1.jpg?profile=product_image)
![Immunofluorescence - Anti-Bcl-6 Antibody [PCRP-BCL6-1D3] (A277775)](https://cdn.antibodies.com/image/catalog/277/A277775_2.jpg?profile=product_image)
![IHC - Recombinant Anti-PD1 Antibody [PDCD1/1410R] (A249588)](https://cdn.antibodies.com/image/catalog/249/A249588_1.jpg?profile=product_image)
![Flow cytometry - Anti-PD1 Antibody [EH12.2H7] (APC) (A121900)](https://cdn.antibodies.com/image/catalog/121/A121900_1.jpg?profile=product_image)